What Exactly is Bronchiectasis?
Just want to throw in an update for you, our readers, there has been alot of confusion over what has happened to Abby. Most people, including well trained Paramedics, Nurses and some Doctors, have questioned us in the content we have placed in here.
Some are questioning why we are going on so much about Abbys diagnosis of Bronchiectasis, as this is curable they say.
The confusion … most readers are thinking of is Bronchitis, which for the most part is curable or at worst manageable.
Bronchiectasis is not curable but can be managed to reduce symptoms and complications under the right circumstances – It “is a progressive disease” which does not get better.
This is where our challenges come in, Abby’s condition of Bronhiectasis is not being properly managed by health care professionals, these so called professionals are continuously stone walling us in the name of money.
For ABBY THIS IS NOT CURABLE, under the proper care this is manageable and she could have a chance at long term survival given the proper care, this is why we need a second opinion which we are currently being refused.
In Canada it is supposedly our right to have a second medical opinion without the previous professionals involved to create smoke screens and muddy the waters of reality.
This is why we are determined to get to the Bostons Childrens Hospital: One – for a true second opinion and two – to give Abby the best chance at a decent life full of hope instead of full of fear, which she currrently has grown to understand more than she should have ever had to at her age.
We have been put into a very bad position, one we did NOT create but one that a NURSE DID CREATE, backed and supported by her own employer, the damn hospital and their legal team!
Now we are burdened with a close to impossible task of the right people to listen to us and the right people to care what happens to Abby – The NS Health Authority does not care about Abby!
Understanding Non-Cystic Fibrosis Bronchiectasis
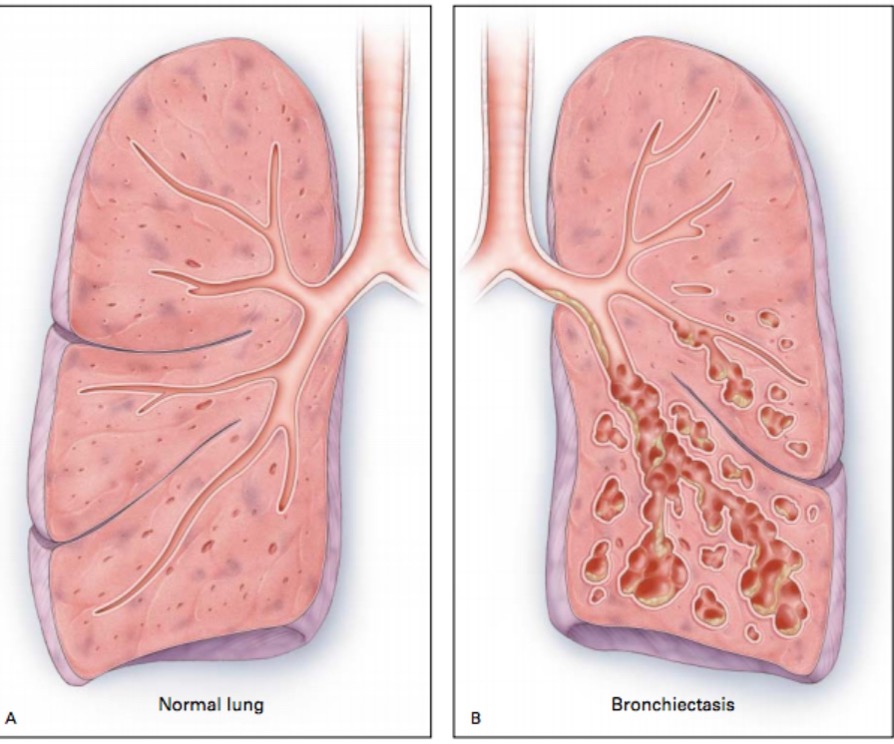
Non-Cystic Fibrosis Bronchiectasis (Non-CF Bronchiectasis) is a lung condition that affects the airways, which are the tubes that carry air in and out of your lungs. In a healthy person, these airways are smooth and clear, allowing air to move freely. However, in someone with bronchiectasis, these airways become damaged, widened, and scarred over time.
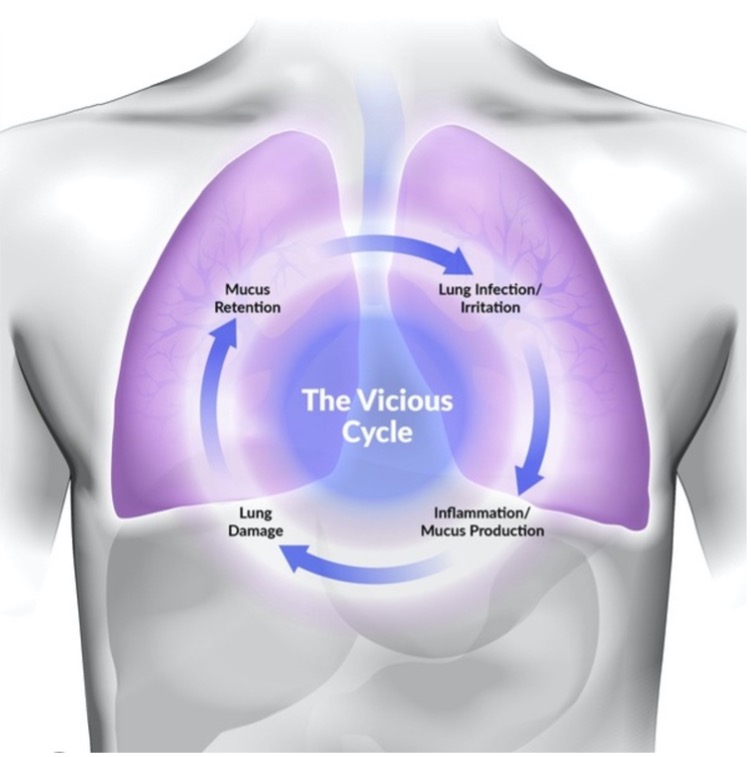
This damage makes it difficult for the lungs to clear out mucus, a sticky substance that the body naturally produces to trap and remove dirt and germs from the airways.
When mucus builds up in the airways and isn’t cleared out properly, it can cause repeated lung infections. These infections can lead to even more damage to the airways, creating a vicious cycle that makes it harder and harder for the person to breathe over time.

What Causes Non-CF Bronchiectasis?
Unlike Cystic Fibrosis (CF), which is a genetic condition that can lead to bronchiectasis, Non-CF Bronchiectasis can be caused by several different factors. Some common causes include:
• Infections: Severe lung infections, such as pneumonia or whooping cough, can damage the airways and lead to bronchiectasis.
• Immune System Problems: Some people have immune system issues that make it harder for their body to fight off infections, leading to repeated lung infections and bronchiectasis.
• Obstructions: Inhaling objects, like a small toy or food, can block the airways and cause damage, potentially leading to bronchiectasis.
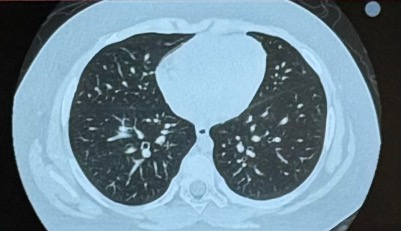
In Abby’s case, the initial cause of her bronchiectasis was a mucus plug—a blockage in the airway that went unnoticed by her medical team in 2019. This blockage led to severe lung damage, which has now developed into bronchiectasis.
Symptoms of Non-CF Bronchiectasis
People with bronchiectasis may experience a range of symptoms, including:
• Persistent Cough: A cough that doesn’t go away, often accompanied by the production of thick mucus (sputum) that may be discolored (yellow or green).
• Frequent Lung Infections: These infections may cause symptoms like fever, fatigue, and increased mucus production.
• Shortness of Breath: Difficulty breathing, especially during physical activities or even simple tasks.
• Chest Pain: Discomfort or pain in the chest area, often due to constant coughing.
• Fatigue: Feeling unusually tired or weak, as the body uses more energy to fight infections and deal with breathing difficulties.
• Wheezing: A high-pitched whistling sound when breathing, especially when exhaling.
Complications of Non-CF Bronchiectasis
If bronchiectasis isn’t managed properly, it can lead to several serious complications:
• Repeated Lung Infections: Because the airways are damaged, they can’t clear out mucus effectively. This creates an environment where bacteria can thrive, leading to frequent lung infections. These infections can cause further damage to the airways, making the condition worse over time.
• Chronic Respiratory Failure: Over time, as the lung damage becomes more severe, the lungs may struggle to provide enough oxygen to the body or remove carbon dioxide. This can lead to chronic respiratory failure, a serious condition that requires long-term medical support, such as oxygen therapy.
• Hemoptysis (Coughing Up Blood): In some cases, the damaged airways may bleed, leading to coughing up blood. While this can be frightening, it’s important to seek medical attention if it happens.
• Fatigue and Weakness: The body uses a lot of energy to fight infections and manage breathing difficulties, which can lead to persistent fatigue and weakness. This can make it difficult for a person to carry out daily activities, leading to a reduced quality of life.
• Heart Problems: Chronic lung diseases like bronchiectasis can increase pressure in the arteries between the heart and lungs. Over time, this can put a strain on the heart, leading to heart problems such as right heart syndrome and pulmonary hypertension (high blood pressure in the lungs).
• Declined Lung Function: Over time, the repeated infections and chronic inflammation associated with bronchiectasis can cause the lungs to become more and more damaged. This progressive damage can lead to a significant decline in lung function, making it increasingly difficult for the person to breathe. As lung function decreases, even simple activities like walking or climbing stairs can become exhausting. This decline can severely impact a person’s quality of life and limit their ability to live independently.
• Death: In severe cases, bronchiectasis can lead to life-threatening complications. As lung function continues to decline, the risk of respiratory failure increases. Respiratory failure occurs when the lungs can no longer provide enough oxygen to the body or remove carbon dioxide effectively, which can be fatal without immediate medical intervention. Additionally, the strain that chronic lung disease places on the heart can lead to heart failure, another potentially fatal complication.

Managing Non-CF Bronchiectasis
The goal of managing bronchiectasis is to control symptoms, prevent complications, and improve quality of life. However, without proper management, the condition can lead to serious and life-threatening complications, including declined lung function and even death:
• Airway Clearance Techniques: These are exercises or devices that help loosen and clear mucus from the lungs. For example, a person may use a handheld device that creates vibrations to help shake mucus loose, making it easier to cough up.
• Medications: Doctors may prescribe antibiotics to treat or prevent infections, inhalers to help open the airways, and other medications to reduce inflammation in the lungs.
• Vaccinations: It’s important for people with bronchiectasis to stay up-to-date on vaccinations, especially for flu and pneumonia, to help prevent infections that could worsen their condition.
• Oxygen Therapy: In more severe cases, a person may need supplemental oxygen to help them breathe better.
• Surgery: In very rare cases, surgery may be needed to remove severely damaged parts of the lung. However, this is usually only considered when other treatments haven’t worked.

Living with Non-CF Bronchiectasis: Abby’s Daily Battle
For Abby, living with Non-Cystic Fibrosis Bronchiectasis is an ongoing challenge that impacts every aspect of her life. This condition has turned what should be the carefree days of childhood into a daily struggle for breath and well-being.
Each day, Abby faces fatigue, weakness, and respiratory distress. Simple activities that other children take for granted—like laughing with friends, running outside, or enjoying a favorite treat—can quickly lead to severe coughing fits and breathing difficulties. These episodes often require immediate medication to help her airways open up and allow her to breathe more easily.
The constant threat of infections looms over Abby’s life. Her damaged lungs are unable to clear mucus effectively, making her highly susceptible to repeated lung infections. These infections not only cause her discomfort and illness but also have the potential to further damage her already fragile lungs, accelerating the decline in her lung function.
To protect her from these risks, Abby’s environment at home is carefully controlled. Non Medical grade Air purifiers run constantly to reduce the presence of airborne irritants and other contaminants that could trigger an exacerbation of her condition. Abby requires Medical Grade Air purifier, however, they are $2,000 per unit. Abby is homeschooled to minimize her exposure to illnesses that could be life-threatening for her. Despite these precautions, the fear of what could happen if she contracts a virus or infection is a constant concern for her and her family.
Abby’s condition also means that she has to endure frequent medical appointments and treatments. The use of medications, while necessary to manage her symptoms, comes with its own set of challenges, including potential side effects that impact her quality of life. Her mother, Adrienne, has to carefully balance the use of these medications, only administering them when absolutely necessary to avoid further complications and avoid overusing Antibiotics.
Despite all these challenges, Abby remains incredibly resilient. She continues to dream of the day she can visit Disney World and meet Cooper Alan, even as she battles a condition that has already taken so much from her. Abby’s fight is not just against her illness but also against the limitations it places on her ability to enjoy the simple joys of childhood.
Living with Non-CF Bronchiectasis means that Abby’s life is filled with uncertainties, but with the right support, she and her family are determined to manage her condition and give her the best quality of life possible.